Having a child with developmental coordination disorder (DCD) is challenging and learning how to support them and their families is a journey indeed. Along the way, you will learn about what it is, the symptoms, treatment options, and professionals who can help.
What is developmental coordination disorder (DCD)?
A term used to describe children who demonstrate substantial difficulty in coordinating movements such as those needed to climb the playground, catch balls, complete handwriting tasks or get dressed.
As a result, these movement difficulties interfere with a child’s ability to perform everyday tasks and have an impact on academic achievement.
DCD is also referred as;
- Clumsy
- Perceptual-motor difficulties
- Motor learning deficit
- Minimal brain dysfunction
- Deficits in Attention
- Motor Control and Perception (DAMP)
- Dyspraxia – You might hear people using the term ‘dyspraxia’ as well as terms like DCD. Dyspraxia means difficulty with movement. It’s symptom of DCD, but isn’t the same as DCD.
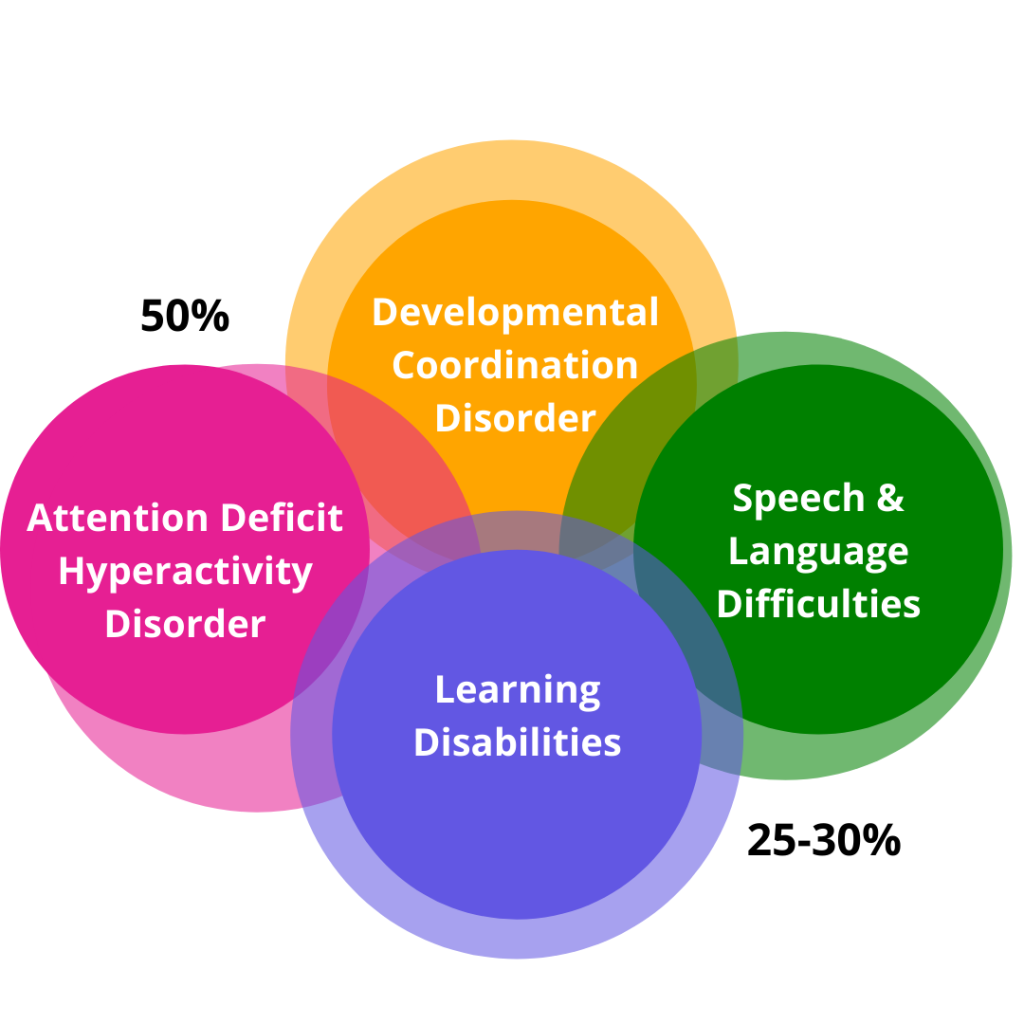
Significant Co-morbidity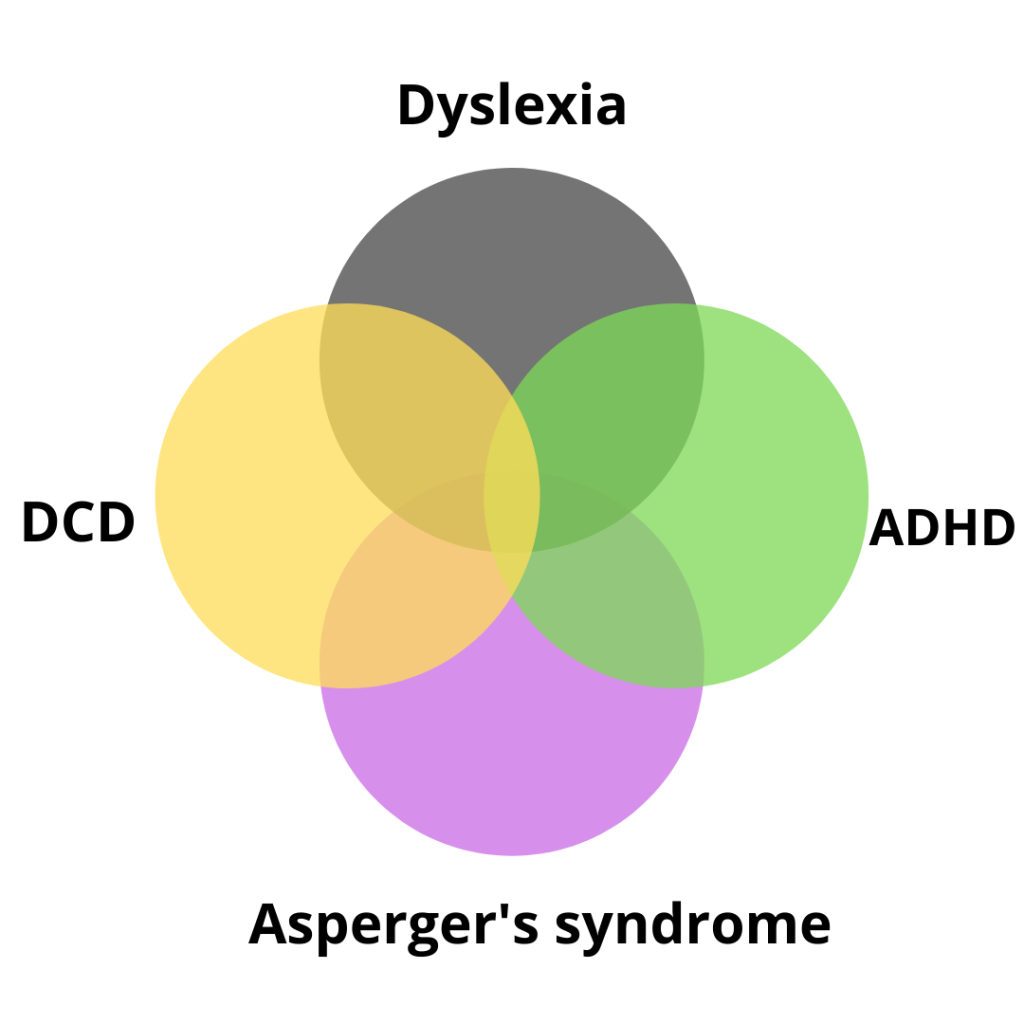
Prevalence:
- Up to 4-5 children/100 will have DCD
- Boy: Girl ratio of 2:1
DSM-IV referred DCD as;
- Marked impairment of the development of motor co-ordination
- Impairment significantly interferes with academic achievement of activities if daily living
- Problem not due to a recognised medical condition (such as CP)
- Not a pervasive developmental delay
Most of the time there are co-occuring conditions associated with DCD. And these are:
- Up to 50% of children with DCD may meet the diagnostic criteria for ADHD (Kadejo & Gillberg 1999; Waterberg et al., 2007)
- DCD frequently co-occurs with learning disabilities (O’Hare & Kalid, 2002; Visser, 2003)
- Specific language impairment has also been associated with DCD (Archibald & Alloway, 2008; Hill, 2001)
- Since the DSM-5, children with ASD may have a co-occuring DCD diagnosis; co-occurence is unknown but >50% of children with ASD may have motor difficulties (Provost et al. 2007)
It can be harder to diagnose DCD in children under 5 years because movement skills vary a lot among children in this age group.
If a child is under 5 years and you’re concerned about their movement, I always recommend a visit to the GP as a first point of contact.
DCD Red Flags:
- Appears clumsy or awkward (e.g. running awkwardly or holding scissors awkwardly).
- Poor body awareness: Trouble determining the distance between themselves and objects and hence bumping into objects or knocking things over and invading other people’s personal space without recognising this.
- Delayed gross & fine motor skills.
- Movement planning difficulties: planning physical movements into a controlled sequence to complete a task.
- Movement learning difficulties: Difficulty learning new movement skills and once learned in one environment (e.g. school) may continue to have difficulty performing the task in another environment (e.g. home).
- Difficulty with activities that require constant changes (e.g. baseball, tennis).
- Difficulty with activities that require the coordinated use of both sides of the body (e.g. cutting with scissors, running, swinging a bat).
- Reduced strength and endurance → more effort to complete the same task as their friends → rapid fatigue.
- Rushing through tasks as completing them slowly is difficult due to reduced control or balance.
- Difficulty with academic subjects such as mathematics, spelling or written language which require handwriting to be accurate and organised on the page.
- Difficulties organising their school desk, school bag, homework or even the space on a page → self esteem
There are common difficulties often (but not always) experienced by the child with Developmental Coordination Disorder (DCD):
- Lack interest/motivation in physical activity.
- Avoid socialising with peers.
- Frustrated easily when completing tasks.
- Easily distracted
- Reduced self-esteem
- Anxiety when asked to participate in difficult activities.
- Tends to seek out younger children to play with as their skills are of a similar level and they feel more confident playing with them.
- May complain that ‘this is too hard’ or ‘I can’t do it’ when presented with motor activities.
- May be resistant to changes in how or when tasks are done as changes present new situations/tasks that require planning and new learning.
Management strategies that support the child with Developmental Coordination Disorder (DCD) (at preschool, school and/or home):
- Encouragement to persist and attempt tasks.
- Provide opportunities to succeed by simplifying activities.
- Teach new skills in a step by step manner and keep the environment as predictable as possible during teaching.
- Introduce new skills on an individual basis before introducing peers.
- Use simple language and instructions.
- Provide visual as well as verbal cues.
- Provide extra time to complete tasks.
- Recognise and reinforce the child’s strengths.
- Set realistic and achievable goals for all task performance and completion.
- Make participation, not competition, the goal.
- Observing the child during play and formal assessment to determine the child’s abilities with gross motor (whole body) tasks and then making recommendations for management.
- Setting functional goals in collaboration with the child, parents and teachers so that therapy has a common focus beneficial to everyone involved.
- Providing ways/ideas to promote physical activity and participation in team/group activities.
- Developing the underlying skills necessary to support whole body (gross motor) and hand dexterity (fine motor) skills, such as providing activities to support balance and coordination, strength and endurance, attention and alertness, body awareness, and movement planning
- Building self-confidence to enable a child to willingly participate (it is common for these children to shut down when they perceive the task to be too hard) in activities by:
- Providing the child with education about why they may be experiencing difficulties with movement, their strengths as well as their weaknesses.
- Breaking down specific physical skills into one or two step components to teach the skill and then gradually adding in new components until the skill is doable in its entirety (e.g. skipping – start with a step, then a hop)
- Presenting the activities at the ‘just right challenge’ level to provide success and then gradually increasing the demands of a mastered skill.
- Improving sensory processing to ensure appropriate attention and arousal to attempt the tasks as well as ensuring the body is receiving and interpreting the correct messages from the muscles in terms of their position and relationship to each other.
- Modelling tasks visually and using hands-on adjustment techniques to aid body awareness for the child.
- Multi-sensory approach: Using a multi-sensory approach to learning new skills (our favourite)
If you feel that your student, child or family member has DCD, you may reach out to us at (02) 4959 8920 or admin@happydots.com.au. We also provide parent/teacher seminars which can be held at one of our clinics or at your school/establishment.



